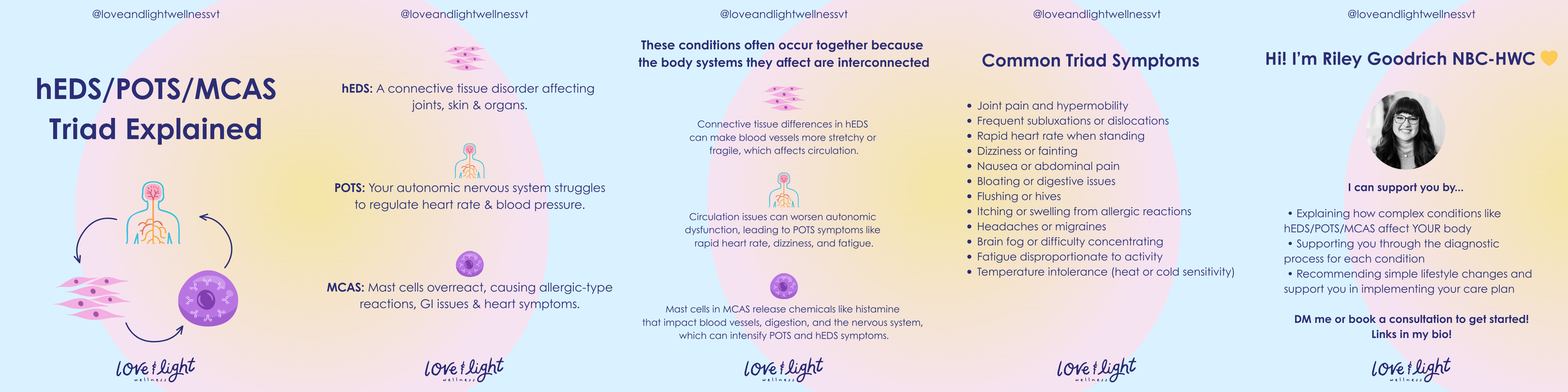
The hEDS/POTS/MCAS Triad
Understanding the hEDS–POTS–MCAS Overlap
If you’ve been diagnosed with hypermobile Ehlers-Danlos syndrome (hEDS), Postural Orthostatic Tachycardia Syndrome (POTS), or Mast Cell Activation Syndrome (MCAS)—or you suspect one of them—you may have noticed something important:
These conditions rarely show up alone.
Many people live for years with confusing, shifting symptoms before realizing they’re experiencing an overlap of connective tissue, autonomic nervous system, and immune dysregulation. This post breaks down what each condition is, why they commonly coexist, and what this means for diagnosis, care, and daily life.
What Is hEDS?
Hypermobile Ehlers-Danlos syndrome (hEDS) is a connective tissue disorder affecting collagen—the protein that provides structure and stability throughout the body.
Because connective tissue is everywhere, hEDS is not just about joint hypermobility.
Common features include:
Joint hypermobility, instability, and frequent subluxations
Chronic pain and early-onset musculoskeletal issues
Fragile or stretchy skin
Poor wound healing or easy bruising
Fatigue and exercise intolerance
Connective tissue also plays a key role in blood vessels, the gastrointestinal tract, and organ support, which helps explain why people with hEDS often experience symptoms far beyond their joints.
What Is POTS?
Postural Orthostatic Tachycardia Syndrome (POTS) is a form of dysautonomia—a disorder of the autonomic nervous system.
POTS is characterized by an abnormal heart rate increase upon standing, but its impact is much broader.
Common symptoms include:
Rapid heart rate, palpitations, or dizziness when upright
Lightheadedness or fainting
Brain fog and cognitive fatigue
Heat intolerance
Exercise intolerance
Gastrointestinal symptoms
Adrenaline surges or anxiety-like sensations
In people with hEDS, lax connective tissue can affect blood vessel tone, allowing blood to pool in the lower body when standing. This can worsen or directly contribute to POTS symptoms.
What Is MCAS?
Mast Cell Activation Syndrome (MCAS) involves inappropriate or excessive activation of mast cells—immune cells involved in allergic responses, inflammation, and tissue repair.
Unlike classic allergies, MCAS reactions may occur without a clear trigger and can affect multiple systems at once.
Common symptoms include:
Flushing, itching, or hives
Gastrointestinal distress (nausea, diarrhea, cramping)
Food and medication sensitivities
Headaches or migraines
Blood pressure changes
Shortness of breath or throat tightness
Fatigue and brain fog
Mast cells live in connective tissue and interact closely with the nervous system—making MCAS particularly relevant in people with hEDS and POTS.
Why Do hEDS, POTS, and MCAS So Often Coexist?
1. Shared Connective Tissue Dysfunction
Connective tissue abnormalities in hEDS can:
Reduce blood vessel stability → contributing to POTS
Alter the environment mast cells live in → promoting inappropriate activation
2. Nervous System–Immune Crosstalk
The autonomic nervous system and immune system constantly communicate. Dysregulation in one can amplify dysfunction in the other, creating a feedback loop of symptoms.
3. Mast Cells and the Nervous System
Mast cells release mediators (like histamine and prostaglandins) that can:
Affect heart rate and blood pressure
Increase nerve sensitivity
Worsen orthostatic intolerance
This means MCAS flares can directly intensify POTS symptoms.
4. Diagnostic Fragmentation
These conditions are often treated in isolation by different specialists. Without a whole-body lens, the underlying pattern may be missed—leading to delayed or incomplete diagnosis.
What the Overlap Feels Like in Real Life
People with the hEDS–POTS–MCAS triad often describe:
Symptoms that shift day to day
Reactions that seem disproportionate or unpredictable
Feeling dismissed because tests look “normal”
Needing to manage posture, food, stress, temperature, and pacing simultaneously
This is not a failure of resilience—it’s a reflection of complex, multi-system physiology.
Why a Whole-Body, Systems-Based Approach Matters
Because these conditions influence one another, care is most effective when it is:
Interdisciplinary (rather than siloed)
Symptom-pattern–based, not just test-based
Nervous-system informed
Pacing- and capacity-focused, not push-through
Support may include a combination of:
Autonomic regulation strategies
Joint stabilization and safe movement
Mast cell–aware nutrition and medication planning
Stress and sensory load management
Education and self-advocacy support
You’re Not “Too Complex”
If you live at the intersection of hEDS, POTS, and MCAS, your body isn’t broken—it’s communicating.
Understanding the overlap helps:
Reduce self-blame
Improve diagnostic clarity
Support more sustainable care plans
Validate lived experience
Healing doesn’t mean fixing everything at once. It means learning how your systems interact—and responding with curiosity, compassion, and appropriate support.
If you’d like help navigating this overlap, building a sustainable care plan, or understanding your symptoms through a nervous-system–informed lens, you don’t have to do it alone. Book a free consultation with me to see if working together can help you make progress in your health journey!